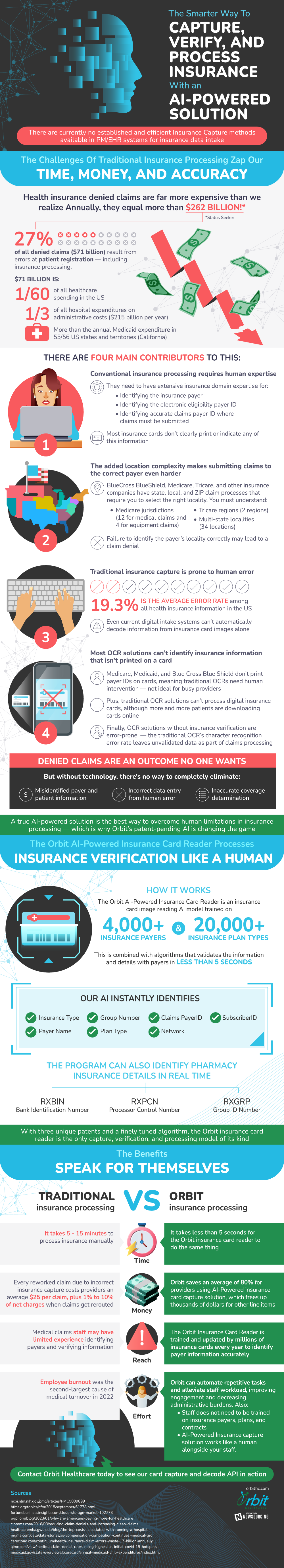
Currently in the health insurance space, many claims are getting denied. In fact, there is more than $262 billion annually that is spent on denied claims; $71 billion of this is due to errors made very early on in the submission process, at the patient registration state. Many of these mistakes are due to the overreliance on manual entry in the traditional insurance procedures. Right now, human input is necessary because it takes a great deal of domain knowledge to know how to locate necessary information that isn’t printed on insurance cards. However, one small mistake or misrepresentation can lead to a claim being denied.
AI and API insurance card capture technologies are being recognized by experts as a great way to overcome human constraints in insurance processing. They have been trained with vast datasets so that they are primed to recognize identifying information such as Claims PayerID, plan types, and group numbers. This whole process takes AI only five seconds, which is much faster than the manual processing period of five to fifteen minutes. In addition to speed, these AI systems provide significant cost reductions by minimizing the number of claims that have to be reworked, which costs $25 per claim.
Source: OrbitHC

